Primary Therapies
When choosing treatments, those with the highest degree of efficacy should be chosen, not only because those will be most likely to alleviate pain, but also because they may decrease the pill burden and improve compliance.
Biologics
- Monoclonal antibodies (mAbs): Due to their high degree of efficacy, anti-nerve growth factor monoclonal antibodies (anti-NGF mAbs) are considered a first-line therapy for chronic osteoarthritis-related pain (label indication). The once-monthly subcutaneous injection (frunevetmab) decreases daily caregiver burden but does require a monthly trip to the veterinary practice or appointment with a house-call veterinarian. Efficacy in other pain conditions is yet to be established.
Pharmacologic Therapeutics
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Due to their high degree of efficacy, NSAIDs are considered a first-line therapy for most causes of chronic inflammatory pain, but there is no approved NSAID for treatment of chronic pain in cats in the United States. However, both meloxicam and robenacoxib are approved for acute pain use in the United States and for long-term use outside the United States. Guidelines have been published for their off-label use (ISFM/AAFP NSAID Guidelines).
- Gabapentinoids: Gabapentinoids (gabapentin, pregabalin) can provide mild to moderate analgesia for some patients, but are best used as part of a multimodal protocol. Based on pharmacokinetic studies, gabapentin should be administered three times/day in most patients. Pregabalin is a potential alternative to gabapentin and is effective when given two times/day. Gabapentin is a Class V scheduled drug in many US states and pregabalin is a Class V in all US states. Since fear-anxiety can exacerbate pain, drugs with anxiolytic effects, such as gabapentinoids, may play a role in decreasing the intensity of pain. Veterinary professionals should be aware of the regulations in their geographic location.
- N-methyl-D-aspartate (NMDA): NMDA receptor antagonists (ketamine and amantadine) decrease central sensitization by blocking the NMDA receptor in the spinal cord. NMDA receptor activity is an important driver of central sensitization, and therefore persistent pain states. Ketamine and amantadine decrease NMDA receptor activity and decrease the amount of central sensitization and thus the level of pain. These drugs may be used as part of a multimodal protocol that includes NSAIDs or anti-NGF mAbs. Despite the widespread use of low-dose SQ ketamine, there is no evidence currently to support this practice.
- Opioids: Opioids are not recommended for treatment of chronic pain as they are less effective than other drugs used for chronic pain. The side effects of long-term opioid use can cause conditions that negatively impact patient health (e.g., anorexia, constipation). There are also valid concerns regarding human diversion and abuse of veterinary-dispensed opioids. They can be considered for treatment of acute breakthrough pain in chronic pain conditions (e.g., flare of chronic pancreatitis pain).
Other Drugs
- Injectable ‘chondroprotectants’: Injectable agents such as polysulphated glycosaminoglycans (PSGAGs) are often used. Evidence for an analgesic effect in cats is lacking, although there is some evidence of an analgesic effect of PSGAGs in other species.
At the time of publication (2023), no drugs listed are licensed for chronic pain treatment in cats in the United States, except the anti-nerve growth factor monoclonal antibody and it is only approved for the treatment of osteoarthritis. In the United States, no NSAIDs are approved for more than three days of treatment, which means they are only approved for acute pain, but both robenacoxib and meloxicam are licensed in some other countries for treatment of chronic musculoskeletal pain. The combined long-term use of an anti-nerve growth factor monoclonal antibody and NSAIDs in cats requires further research.
Nutritional Supplements
- Nutritional supplements, including so-called oral chondroprotective substances, are often used in the hope they will assist in the management of pain
- Currently, there is very little evidence to support their efficacy in painful conditions.
- Diets enriched in omega-3 fatty acids are thought to provide mild to moderate pain relief for joint pain, and there is interest in harnessing the analgesic potential of unique combinations of fatty acids, especially marine-based fatty acids.
Non-pharmacologic Therapy
- Integrative medicine modalities might be considered as part of an integrative plan in many cats. Not all cats are amenable to non-pharmacologic therapy options, and repeat visits to the veterinary practice for treatments are necessary for most modalities. Evidence-based medicine supporting the use of these modalities in cats is mostly lacking. Although specific research in cats is limited, the modalities have scientific evidence base in other species. Integrative medicine modalities include physical medicine, traditional Chinese veterinary medicine, nutrition and nutraceuticals, Western herbal medications, and aromatherapy.
Considerations
- Using a multimodal approach, especially if pain is moderate to severe, can provide more profound pain relief since the treatments work at different sites in the pain pathway, or can amplify effects of other treatments even if working at the same site. NSAIDs and anti-NGF mAbs will generally provide analgesia when used alone for mild or moderate pain, and occasionally when used alone in cases of severe pain.
- Consider the patient and caregiver support needed for each therapy in order to reduce stress for both parties. Increasing caregiver burden often results in decreased compliance.
- The caregiver’s budgets of care (financial, time, emotional, and physical) must be considered when creating therapeutic plans, all of which impact the cat and caregiver’s quality of life (QOL), caregiver compliance, and cat-caregiver bond.
- More on environmental modifications can be found under the Patient Support tab of this Toolkit.
Tiered Approach
The figure below outlines a tiered approach to pain management. Tiers are presented from the highest recommendation (most evidence) to the lowest.
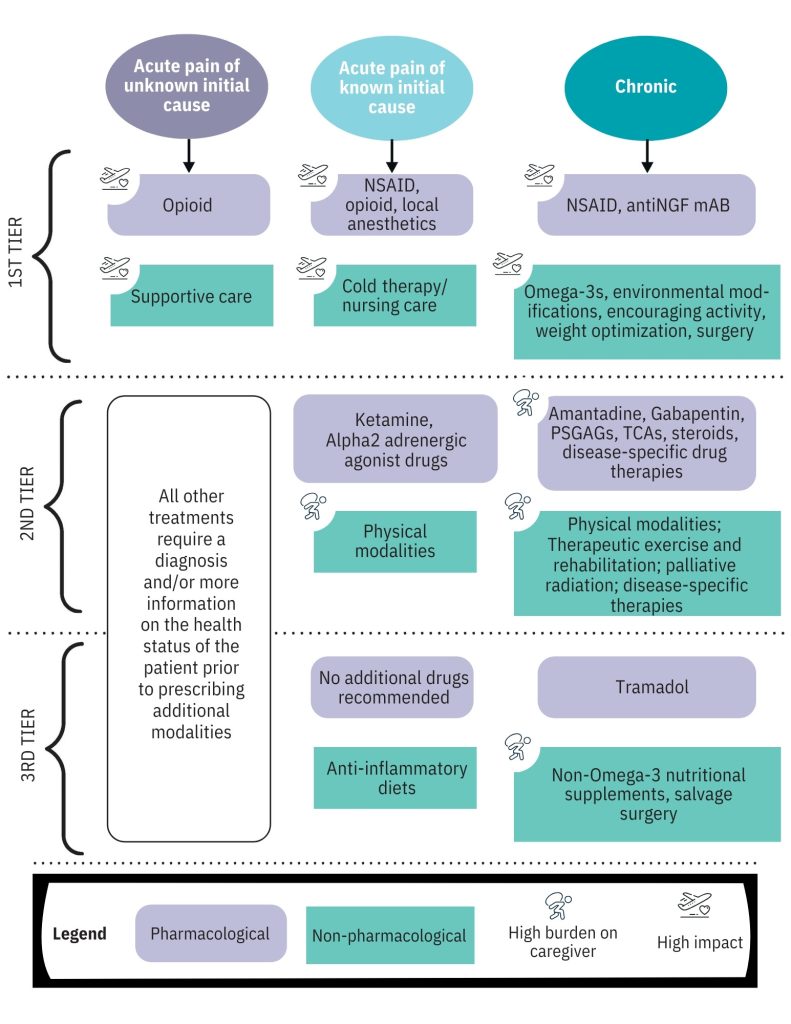
aAdapted from Gruen ME, Lascelles BDX, Colleran E, et al. 2022 AAHA Pain Management Guidelines for Dogs and Cats. Available here.
